Toxoplasma
(Toxoplasma gondii)
Toxoplasma gondii is an apicomplexan that infects domestic and wild felids (definitive hosts) and a wide range of intermediate hosts (e.g. small birds and mammals, including felids). It is zoonotic.
Distribution
Worldwide
Clinical signs
Toxoplasma gondii rarely causes clinical disease in cats. Initial infection may produce diarrhoea in young animals. As cats themselves act as intermediate hosts to the parasite, immunosuppressed cats may display clinical signs depending on the location of the tissue cysts. Common signs include fever, anorexia, uveitis, iritis, iridocyclitis, chorioretinitis, pneumonia, hepatitis, hyperaesthesia from polymyositis, and ataxia, circling, behavioural changes, seizures and tremors from nervous system infection [1,2]. Clinical toxoplasmosis is most severe in neonates infected in utero or during lactation, leading to life-threatening, poly-systemic disease.
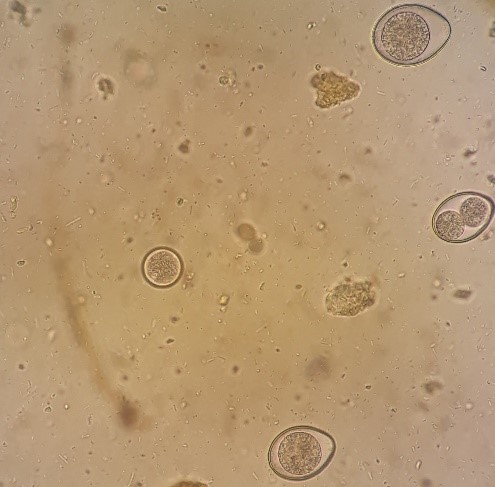
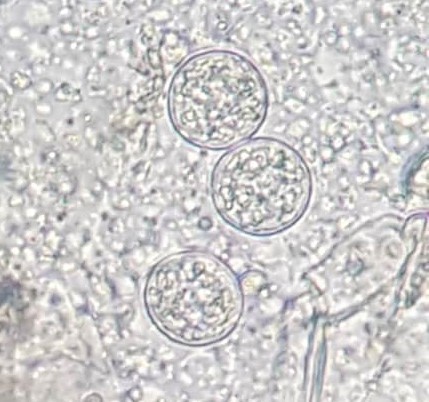
Figure 1. Oocysts of Toxoplasma gondii and Cystoisospora rivolta (A) and oocysts of T. gondii (B) from the faeces of a cat by faecal flotation (Image credit: Dr. B. K. Linh, Dr. M. Watanabe)
Diagnosis
Because cats only shed T. gondii oocysts (10 x 12 µm) [1] for 1-3 weeks after their first exposure (Fig. 1), oocysts are rarely found in faeces by standard faecal flotation (SOP 1). Serological tests may be useful to determine if the cat is negative (thus, susceptible to infection) and positive (and whether it is a recent/active or past infection). Systemic, extra-intestinal infection may be diagnosed by serology (high IgG titres) or via detection of parasite DNA e.g. cerebrospinal fluid or bronchoalveolar lavage. Concurrent immunosuppression with Feline Infectious Peritonitis, Feline Immunodeficiency Virus and Feline Leukaemia Virus commonly predispose to systemic toxoplasmosis as a result of recrudescence of latent infection
Treatment
Off-label use of clindamycin hydrochloride (10-12 mg/kg PO twice daily for 4 weeks) or clindamycin phosphate (12.5-25 mg/kg IM twice daily for 4 weeks) are reputed to be effective for treating clinical toxoplasmosis in cats. For ocular lesions, topical corticosteroids and atropine may be of additional benefit [2].
Prevention and Control
Cats should not be fed raw or undercooked meat, should be kept indoors and should not be allowed to hunt. The litter box should be changed daily; pregnant women and immunosuppressed individuals should not change litter to avoid the potential transmission of Toxoplasma through ingestion of sporulated oocysts.
Public health considerations
Toxoplasma gondii is zoonotic and can cause severe disease in humans. Congenital infection may occur in women that are infected for the first time during pregnancy or that are immunocompromised. Immunocompromised individuals (e.g. infected with HIV / AIDs or on immunosuppressive drugs) are also at increased risk of toxoplasmosis (either from previously latent or newly acquired infection).
Direct contact with cats is not a direct risk factor for T. gondii infection in humans, especially if faeces is removed from litter trays on a daily-basis as oocysts take at least 2-3 days to become infective [2]. Ingestion of contaminated food (e.g., raw or undercooked meat, unwashed fruits and vegetables) or soil is the most common source of infection in humans. Prevention can be exercised by avoiding consumption of raw or undercooked meat, by washing hands and food preparation surfaces with warm soapy water, by wearing gloves while gardening or washing hands after gardening. Fruits and vegetables should also be washed thoroughly before eating.
References
[1] Bowman DD, Hendrix CM, Lindsay DS, Barr SC. Feline Clinical Parasitology. Iowa State University Press, Ames, USA. 2002.
[2] Davidson MG. Toxoplasmosis. Vet Clin North Am Small Anim Pract. 2000;30:1051-1062.
[3] Dubey JP, Ferreira LR, Martin J and Jones J. Sporulation and survival of Toxoplasma gondii oocysts in different types of commercial cat litter. J Parasitol. 2011;97:751-754.
